Trauma and Emotional Dysregulation

Traumatic reactions hit out of the blue, coming from nowhere. These responses don't feel caused by a thought or a particular way of thinking. They feel out of control and overwhelming.
If you've experienced significant trauma, you've probably felt deeply discouraged by the advice you receive. The tools and techniques shared for emotional regulation—whether in therapy, educational videos, or self-help resources—can seem almost irrelevant, or at best, far too simplistic. The cognitive behavioral therapy cycle, relied upon heavily in therapeutic contexts, feels disconnected from your lived reality.
Today I want to explain how trauma causes emotional dysregulation and I'll explain what happens in our body and mind when we experience trauma. Memories are stored differently in ways that impact emotional dysregulation indefinitely until you can heal, process, and resolve the traumas.
I also want to share the hope that this healing is possible and I'll discuss how to adapt typical suggestions for yourself if you've experienced significant trauma.
Understanding Traumatic Events
A traumatic event is one in which a person is threatened physically, emotionally, or spiritually in a way that presents a survival threat.
This can also apply to a threat to personhood, .particularly for children who are developing their sense of self, which is closely tied to their caregivers. Neglect and emotional abuse can have very long-lasting impact.
Not all trauma is major physical abuse, war, or actual exposure to death, which is how trauma used to be defined. The definition is now broader.
With the definition above, trauma causes a person to be emotionally overwhelmed. The situation is beyond their ability to cope. They experience severe emotional dysregulation, which makes sense for the situation. But trauma can also cause ongoing emotional dysregulation.
What Happens in Your Body During Trauma
What happens during a traumatic event is that adrenaline floods your system, enabling you to run, fight, or freeze. Then cortisol kicks in, and the cortisol actually shuts down your hippocampus in a way that prevents the memory of that event from moving into long-term storage. The memory stays in the emotional brain.
When you think about it, this makes sense. In prehistoric times when we lived in a world where physical survival was constantly in question, having threats to our physical survival stay in the emotional brain—in the immediacy and intensity of the emotional brain—served a protective purpose.
Traumatic memories feel very different from other memories.
One crucial aspect of traumatic memories is that they're often stored in fragments—fragments of a smell or a sound. They don't always have a full narrative. The traumatic event is embedded in your emotional memory where sensory information is tied to a physiological response. This has real implications for us on an ongoing basis in terms of emotional regulation.
Another key factor is that our limbic system, our emotional brain, has no sense of time. These memories are stored without a linear sense of time, without any understanding that an event occurred, say, 40 years ago. Time is a concept understood by the cognitive parts of our brain—the frontal lobe.
When these sensory fragments are triggered, your body responds as if that event is happening now.
Intense experiences link the sensory information surrounding the trauma to the emotional response you have during the trauma. This is what becomes a trigger.
These triggers can actually be positive or negative - any experience with an intense emotional impact can cause this. For example, if there's a smell that reminds you of your grandmother who was a positive figure in your life and comforting, that smell might bring up those feelings of comfort and relaxation even 40 years later.
Triggers can work both ways, but they tend to be more intense with negative experiences. When people talk about a trauma trigger or an emotional trigger, this is the link they're referring to.
These links are stronger the more intense the initial experience was and the more often it happened—particularly when you were a child.
The more often the link is reinforced as you're growing up and in your current life, the stronger it becomes.
This happens with either big-T or little-t traumas.
Preverbal memories can also create these links. Preverbal trauma refers to trauma that happened in very early childhood - before the child was verbal or able to think in a linear fashion with a sense of time. Trauma triggers are especially difficult for people who have had preverbal trauma.
They may have no memory of the trauma. They just might have the triggers disrupting their emotional regulation on an ongoing basis.
Why Traditional CBT Feels Irrelevant for Trauma Survivors
The typical cognitive behavioral therapy cycle has been proven to be very effective by considerable research. But for people who have experienced significant trauma, it doesn't feel effective. Let me explain why.
The typical cognitive behavioral therapy cycle has been proven to be very effective by considerable research. But for people who have experienced significant trauma, it doesn't feel effective. Let me explain why.
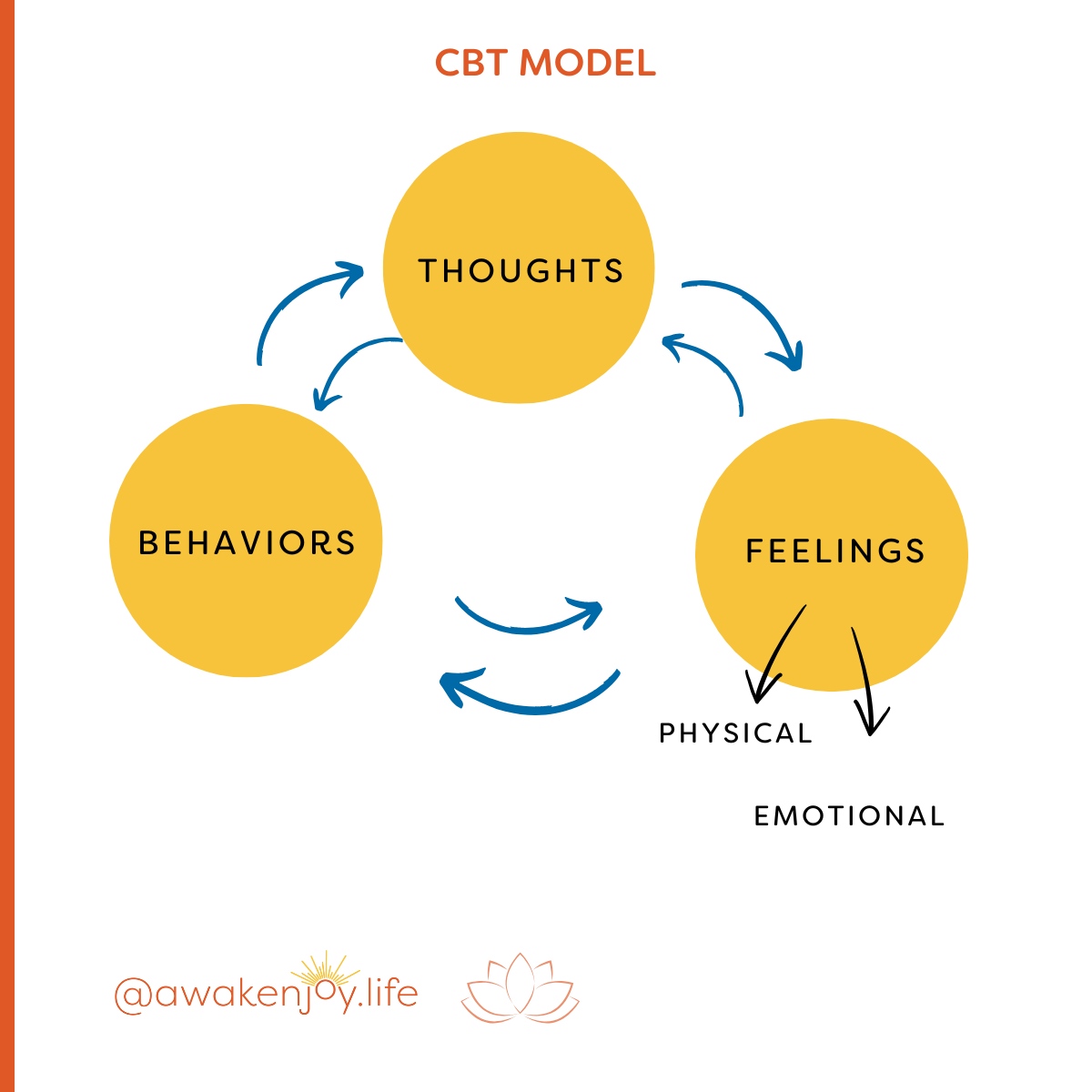
The typical CBT cycle states that our feelings are primarily caused by either our behaviors or our thoughts. It is based on the premise that how we think about something creates an emotional response, and on how behaviors can contribute to the emotional response and the negative thinking.
All these elements interact with each other. How you think impacts how you feel and behave, how you feel impacts your behaviors and your thoughts, and your behaviors impact your thoughts and feelings. They're all connected.
CBT focuses on changing thoughts and behaviors to impact how you feel.
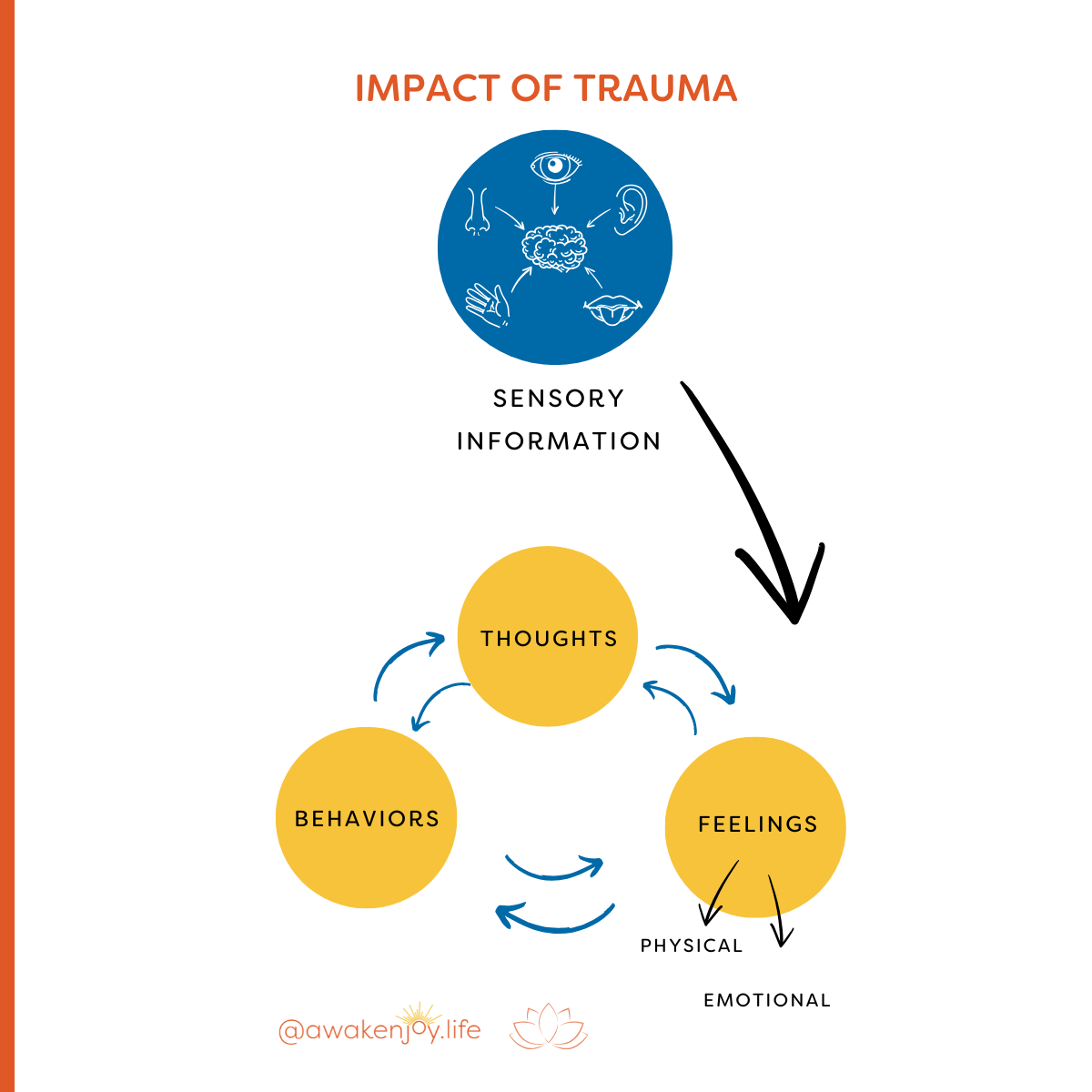
But what happens with someone who's experienced trauma is that the sensory information rushes in and creates the physical and emotional feelings.
The person experiencing that will think, "My thoughts have nothing to do with this. I was triggered before any thought happened." And that is true.
I agree that trauma triggers create the emotional response. The other elements aren't happening—it's not caused by your conscious thoughts. So you can't cure it with your conscious thoughts alone. But let's examine this cycle in a way that might be truly helpful for you.
Adapting the CBT Cycle for Trauma Survivors
A key concept to remember is that you may not be able to stop that initial feeling.
I know you want that initial feeling to stop, but bear with me.
The sensory information comes in. You immediately have dysregulated feelings related to a fight, flight, or freeze response. Common responses include total shutdown, anger, rage, fear, anxiety, and panic. Those are all typical trauma trigger responses.
Let's say you can't stop this initial response.
Then it's helpful to think through what happens after this occurs. After this happens, you might engage in some behavior that isn't helpful in the long run, or you might go down a thought pattern of "What is wrong with me? I'm defective. I'll never get over this."
Either the unhelpful behaviors—which could be drinking or eating too much or screaming and yelling at someone—or the thought patterns will cause other problems down the line. Many different behaviors can come from these feelings that will cause problems later. There are many thought patterns that come from this that all contribute back into the problem.
What I want to encourage you to do initially is this: if these triggers are going to hit you, how do you help the cycle end there? What can you do to intervene at that moment without running to the behaviors that will make things worse or the thought patterns that will escalate all the feelings?
Understanding Your Personal Cycle
A key step is to understand your cycle. Understand what thought patterns—what rabbit hole thoughts—you go down after this happens. Understand what behaviors you engage in that don't serve you and might contribute to the problem.
Once you understand your cycle, bring in the concept of not letting yourself go down those pathways. You can deal with the trigger you're having, but leave it at that. It doesn't go into the rest of the cycle.
Resources for Breaking the Cycle
I have a couple of resources that will help with this, and I'll mention them now before returning to what else you can do when that trauma trigger hits.
Research has shown that trauma causes negative core beliefs to develop, changing your self-image. Knowing your own negative core beliefs is helpful in terms of identifying when you're spiraling down with negative thoughts.
I have a free PDF on identifying your negative core beliefs. This PDF will help you figure out what your core negative belief is. Examples include, "I'm in danger," "I'm defective," "I'm unlovable," "I'm not worthy." The PDF also gives you tools and techniques to begin rewiring those beliefs.
Professional Trauma Treatment Options
Traumatic memory processing with a trauma-informed therapist can be extremely helpful.
Trauma-informed therapy and processing traumatic memories can help them resolve in a way that those trauma triggers don't create such a strong emotional response.
Helpful techniques include trauma-informed cognitive behavioral therapy, somatic-based therapies and EMDR (eye movement desensitization and reprocessing therapy).
When I was actively working as a psychotherapist with trauma survivors, I found EMDR to be the most effective treatment for trauma and anxiety, in most situations. EMDR combines physiological calming techniques with the reprocessing of memories in a way where you can move in and out of the physiological trauma response back into a sense of safety or calm, or at least groundedness in the present.
With any of these techniques, bringing in the sense of being here now—grounded in the present—while also discussing the trauma is essential.
Feelings come up, but then you reground.
Moving between those states while discussing the trauma helps to move it into long-term memory. It can take all of those fragments and turn them into more of a story and more of a long-term memory where you'll think, "Okay, I remember that happened, but I'm not re-experiencing it."
When you reach the point where you're not re-experiencing it, that's probably a point of resolution.
Self-Guided EMDR Option
I know that many of my viewers don't have access to quality therapy or trauma-informed therapy. There is an online resource that can be helpful called
Virtual EMDR.
(Use Promo Code: AWAKENJOY20 for 20% off. The program code must be put into the promo code box when you checkout for the discount! This is an online service I have used and I support!)
I am an affiliate because I do know that this program has helped many people. It's software that assists you in doing self-guided EMDR.
I have a video on whether doing self-administered EMDR is a good idea for you or not, because it's definitely not for everybody.
Daily Practices That Build Resilience
Beyond addressing the cycle and processing trauma, there's something else that can help you enormously: grounding techniques and breathing techniques, if practiced regularly.
Sometimes breathing techniques are not accessible to people who have had trauma. Grounding techniques can be somewhat easier to access, but breathing is excellent if it helps you calm down physiologically.
The key is to practice these techniques not in the middle of being triggered. Practice them when you're in a relatively stable space. The more you practice them, the more access you'll have to them. The more you'll be able to draw on them when you do get triggered.
I recommend that people do diaphragmatic breathing three times a day, five minutes at a time, every day, regularly.
If diaphragmatic breathing doesn't work for you, try grounding techniques. I'll link my videos on these topics here: Diaphragmatic Breathing and Grounding Techniques.
Practicing these regularly is crucial for people with a trauma background.
As you strengthen your ability to access physiologically relaxed—or at least not activated—states, you'll be able to bring them in earlier in this cycle. When that trauma trigger hits, you'll be able to access some of those grounding techniques.
This might not have a huge impact initially, but over time it will have a greater and greater impact on that physiological activation. Again, you may not be able to stop that initial trigger, but you'll be able to calm yourself down more quickly.
Moving Forward with Hope
I hope this has been helpful. This is a very complicated topic. I hope you can give yourself credit for getting through this article and really putting in the effort to heal. Know that this was not your fault, that healing is possible, and be willing to practice and practice and practice. You can get there.
Please let me know what questions you have. I wish you health and healing, and I'll "see you" next week!
Blog Author: Barbara Heffernan, LCSW, MBA. Barbara is a licensed psychotherapist and specialist in anxiety, trauma, and healthy boundaries. She had a private practice in Connecticut for twenty years before starting her popular YouTube channel designed to help people around the world live a more joyful life. Barbara has a BA from Yale University, an MBA from Columbia University and an MSW from SCSU. More info on Barbara can be found on her bio page.
Share this with someone who can benefit from this blog!